What Is an Infant Heel Warmer and Why Is It Used in Hospitals?
When you think about newborn care in hospitals, you might imagine incubators, swaddling blankets, or feeding routines. But tucked into many neonatal units is a small yet essential tool: the infant heel warmer. Though often overlooked by those outside the medical field, this simple device plays a critical role in newborn health assessments, particularly during blood collection.
In this article, we’ll explore what an infant heel warmer is, why it’s used, and what medical experts say about its benefits in hospital settings.
What Is an Infant Heel Warmer?
An infant heel warmer is a small, soft pouch or pad that can be gently wrapped around a newborn’s heel to raise the skin temperature in that area. The warming effect increases local blood flow, making it easier for healthcare professionals to collect a blood sample from the baby’s heel.

Why Hospitals Use Infant Heel Warmers
Facilitating Newborn Blood Tests
One of the most common reasons for using a heel warmer is to aid in heel stick procedures—a method for collecting capillary blood from infants. This technique is frequently used for:
· Newborn screening tests (to detect metabolic or genetic disorders)
· Blood glucose monitoring in infants at risk for hypoglycemia
· Bilirubin testing for jaundice assessment
By warming the heel, blood vessels dilate, and blood flow to the capillaries improves, making the heel stick less traumatic and more efficient.
According to the Medscape, warming the heel for at least 3–5 minutes before puncture can significantly increase sample volume and reduce the need for repeat pricks.
Reducing Pain and Stress
For newborns, any invasive procedure can cause distress. A heel warmer can reduce the time needed to collect the sample, which in turn minimizes discomfort.
A study published in the National Library of Medicine found that pre-warming the heel not only improved blood flow but also shortened collection time by up to 40%, which was associated with lower stress responses in infants.
Improving Sample Quality
Cold extremities in newborns can lead to insufficient or hemolyzed samples, which may compromise test results. Using a heel warmer ensures the blood flows freely, reducing clotting or air bubble issues during micro-sampling.
How an Infant Heel Warmer Works
Activation
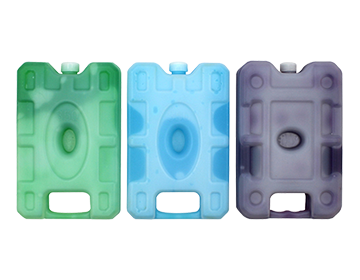
Most modern heel warmers are single-use, disposable packs. They are activated by bending, shaking, or pressing the pouch to trigger a chemical or phase change reaction.
Application
The warmer is gently wrapped or held against the heel for a recommended period—often 3 to 5 minutes—until the skin feels warm to the touch. Care must be taken to avoid overheating or direct skin burns, so devices are designed with temperature limits that prevent exceeding safe skin-contact heat levels.
Safety Features
· Non-toxic materials
· Temperature regulation
· Soft fabric cover to protect delicate skin
Safety Considerations in Hospital Use
Hospitals follow strict protocols for infant warming devices to ensure patient safety. The World Health Organization (WHO) recommends:
· Avoiding temperatures above 42°C (108°F) to prevent skin injury
· Monitoring skin color and condition during warming
· Using heel warmers only for the minimum required time
It’s also important to ensure heel warmers are clean, sterile, and intended for single-patient use to prevent cross-contamination.
Expert Opinions on Heel Warmers
“Heel warming is an essential pre-analytical step for neonatal capillary blood collection. It improves blood flow, reduces collection time, and enhances overall sample quality,” says Dr. Karen S. Thompson, a pediatric pathologist at Children’s National Hospital.
Many nurses and lab technicians agree that heel warmers save time and reduce repeat procedures—critical in busy neonatal intensive care units (NICUs).
Alternatives and Adjuncts
While heel warmers are the most common approach, other warming methods exist, including:
· Warm, moist towels (less consistent temperature control)
· Dry heat lamps (risk of overheating if unsupervised)
· Skin-to-skin contact (for general warming, but less targeted for blood draws)
However, disposable infant heel warmers remain the gold standard due to their safety, portability, and ease of use.
The Bigger Picture: Comfort and Care for Newborns
Using an infant heel warmer is a small but significant example of gentle care in hospital settings. For parents, it’s reassuring to know that medical teams consider both the efficiency of testing and the comfort of their baby.
In many hospitals worldwide, the use of heel warmers has become standard practice, not just because they make blood draws easier, but because they embody a broader philosophy: minimizing stress and pain for the most vulnerable patients.
About INTCO Medical
INTCO Medical provides reliable healthcare solutions worldwide, including high-quality infant heel warmers designed to ensure accurate blood sampling and greater comfort for newborns. With strict international certifications and trusted OEM/ODM capabilities, INTCO supports hospitals and clinics in delivering safer, more effective neonatal care. Partner with INTCO Medical today to bring trusted infant care products to your patients.